Disease primer: Bacterial infections
For an infectious agent, infectivity refers to the proportion of exposed persons who become infected. Pathogenicity refers to the proportion of infected individuals who develop clinically apparent disease. Virulence refers to the proportion of clinically apparent cases that are severe or fatal. The disease process may never progress to clinically apparent illness, or result in illness that ranges from mild to severe or fatal. This range is called the spectrum of disease. Ultimately, the disease process ends either in recovery, disability or death.
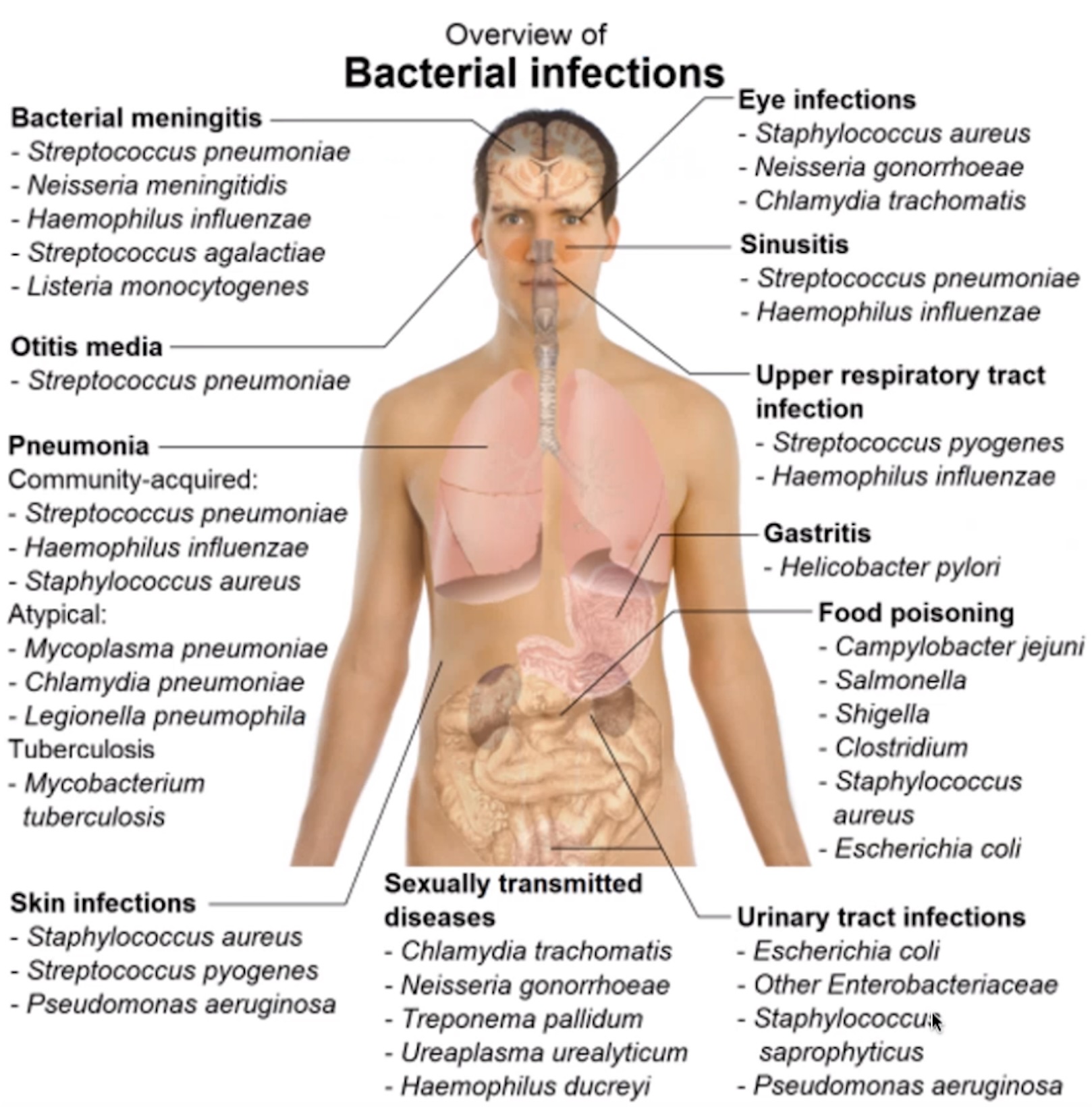
A bacterial infection is classified according to the site of infection, and sometimes also the source of infection.
- Skin
- Lung
- CAP
- Probably Pneumococci, haemophilus influenzae, mycoplasma)
- HAP/VAP
- Probably S.aureus, P.aeruginosa, enterobacteria
- Pseudomonas not in gut, it is found in shower heads or sinks -> can only infect after ABX trt, when gut flora is compromised.
- CAP
- IAI
- BSI
Sepsis
Sepsis is a special life-threatening state. Occurs rarely in UTI, mostly in lung infections.
The SOFA-score is often used to assess organ failure in septic patients.
Septic chock
Septic chock is a development of sepsis that is even more severe.
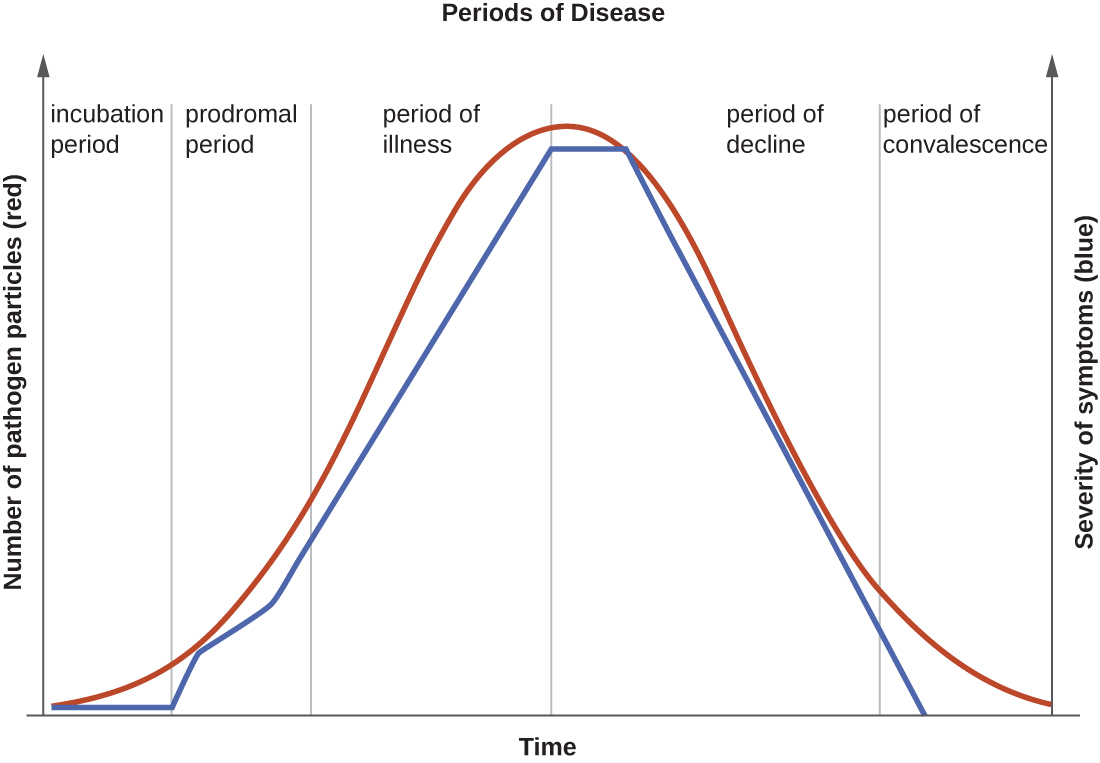
Periods of disease
The progression of an infectious disease can be divided into five periods, which are related to the number of pathogen particles and the severity of signs and symptoms (Figure 2). Infectious diseases can be contagious during all five of the periods of disease.
| # | Period/Phase/Stage | Description |
|---|---|---|
| 1 | Incubation/latency | Pathogen replicates. No signs or symptoms. |
| 2 | Prodromal (subclinical disease) | Pathogeon replicates. General signs and symptoms. Immunesystem active. |
| 3 | Illness (clinical disease) | Most severe and characteristic signs and symptoms. Usual time of diagnosis early in this period. |
| 4 | Decline | Pathogen particle-count declines. Signs and symptoms improve. Immune system possibly weakened—suceptibility to secondary infection. |
| 5 | Convalescence | Patient return to normal function. Signs and symptoms resolve. Some permament damage might have occured. |
Stages might overlap. The onset of symptoms marks the transition from subclinical to clinical disease.
Diagnosis
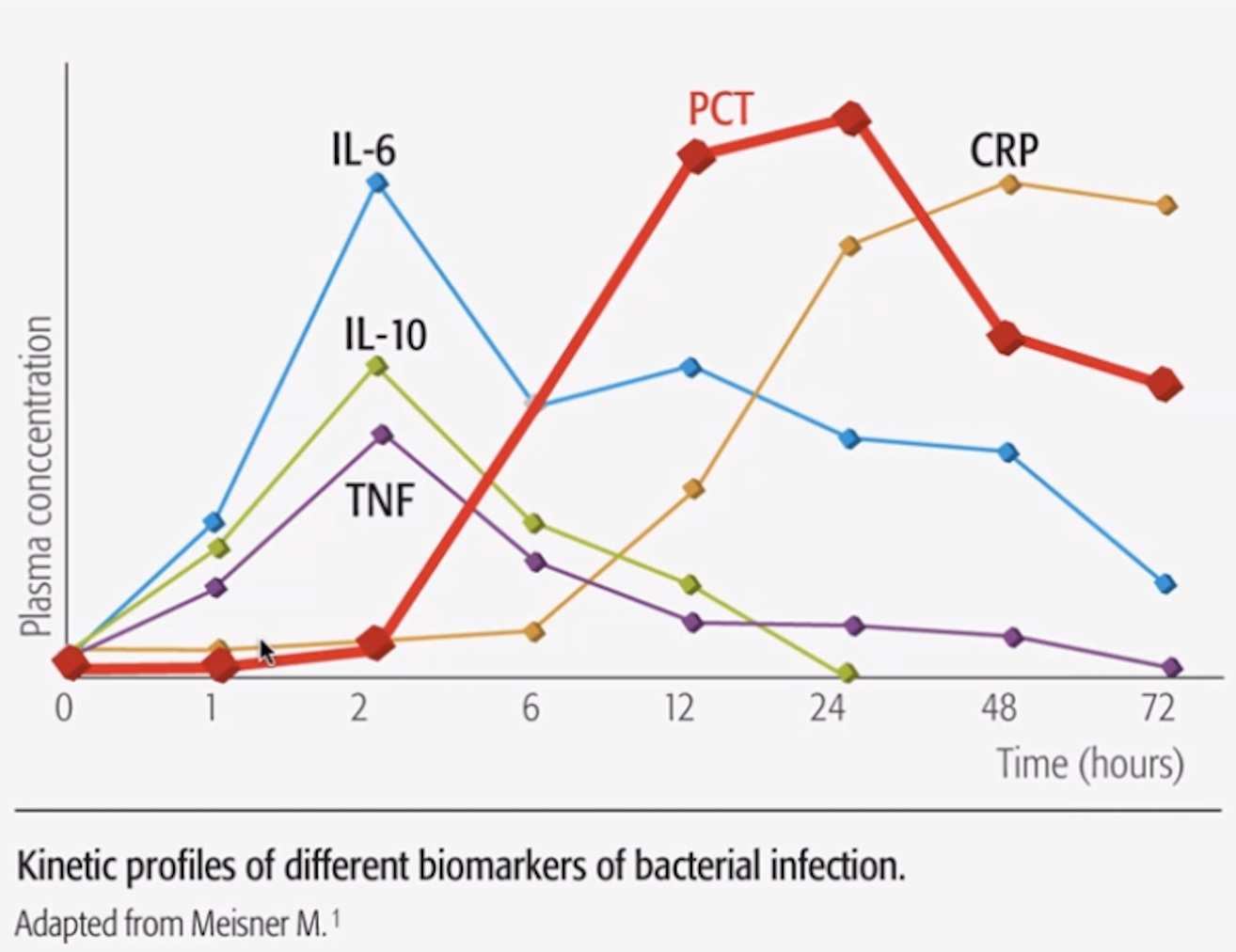
- Biomarkers not specific
- 3 markers + WBC (but unspecific)
- CRP (comes late)
- PCT (quicker than CRP)
- IL-6
- 3 markers + WBC (but unspecific)
- Microbroth
- Accurate + expensive
- Vitek (turbidity), (will be replaced by MALDI-TOF?)
- Not as accurate as microbroth
Treatment
- Efficacy of ABX treatment is judged by signs and symptoms (Are you feeling better than yesterday?), and the course of inflammatory markers (WBC, CRP, PCT)
- Most infections can be treated in 5–7 days
- Right treatment gets 90% success, wrong treatment gets 60% success (“90/60 rule”)
- 95% empirical treatment first (“hit hard and hit early” -Paul Erlich), no time to wait for culture results
- Focus? (sepsis)
- Lung > IAI >> Wounds/UTI
- Where acquired? Immune deficiency?
- “Pneumonia triade”
- Additional risk factors for MDR?
- Co-morbidities?
- Interactions?
- Treatment re-evaluation after 3 days
- 48 h needed to see if ABX works
- Empiric treatment should ideally be switched to targeted treatment once culture results are available (2-3 days)
What we want to know before treating an infection
- Probable infection source
- History
- Examination (lab tests, x-ray, CT-scan)
- Probable bacteria & antibiotic susceptibility
- Medical training
- Local epidemiology
- Individual resistance risk
- Previous infection with resistant bacteria
- Recent travel
- Hospitalization or antibiotics
- Other considerations
- Allergy
- Other drugs (interaction risk)
- Co-morbidities
- PK
Resistance rates: how many are resistant? In percent.
- Clinical dogmas: Foreign body infection -> biofilm
- Immunosuppressive